
The first time you heard the word “diabetes,” you probably also learned about insulin. Your body makes this hormone in an organ called the pancreas. Insulin manages your body’s energy.
Most of the food that you eat is broken down into a type of sugar called glucose. Glucose travels to all the cells in the body through the blood. Insulin allows glucose to leave the blood and enter the cells of the body, where it can be used to create energy. In diabetes, the body is unable to make enough insulin to meet its needs.
With type 1 diabetes, the pancreas can no longer make insulin. People who have type 1 diabetes must inject insulin in order to survive. For good blood glucose control, injections are most commonly done three or four times daily. An insulin pump is another option to deliver insulin.
If you have type 2 diabetes, your pancreas is still able to make some insulin. The beginning stages of type 2 diabetes can often be treated with changes in eating habits, regular physical activity and oral medications. These adjustments allow the body to use the insulin that is being made more effectively.
The longer someone has type 2 diabetes, the less ability the pancreas has to make insulin. Once medications no longer keep blood glucose at a healthy level, insulin must also be used. This might begin with an injection of intermediate or long-acting insulin at bedtime, along with oral medication. As time goes on, injections may be needed throughout the day.
Advances continue to be made in diabetes treatment. Many more options are now available to assist those with diabetes to live in living long, healthy lives. New types of insulin, and new ways to use it, help people with diabetes to keep their blood glucose under control.
Types of insulin
Different types of insulin affect the body in different ways. Each insulin has:
- an onset (amount of time it takes to start working)
- a peak (when it is most effective)
- a duration (how long it works).
Insulin available in Canada today comes in four basic types. These are: rapid, short, intermediate, and long-acting types.
- Rapid-acting insulin begins to work very quickly (in four to 20 minutes). It reaches peak effect in 30 to 120 minutes and stays active for about three to five hours. Since it works so quickly, food must be eaten within 10 to 15 minutes of injecting it. For most people, the peak of rapid-acting insulin matches the highest rise in blood glucose after eating. For this reason, rapid-acting insulin can be very effective in lowering blood glucose after meals.
- Short-acting insulin begins to work in 30 minutes, reaches peak effect in two to three hours, and works for six and a half hours. This type is usually injected 30 to 45 minutes before eating.
- Intermediate-acting insulin begins to work in one to three hours and reaches maximum effect in five to eight hours. It may last for up to 18 hours. This insulin is cloudy and must be gently shaken to re-suspend the insulin before injecting. (It’s important to mix this insulin evenly. See mixing instructions in the “steps for injecting insulin” section below for instructions.)
- Long-acting insulin begins working in 90 minutes. It lasts from 24 up to 42 hours depending on the brand and has a similar effect the entire time it is working. Long-acting insulin, used once or twice daily along with rapid-acting insulin at each meal, gives results very close to the natural action of insulin in someone without diabetes.
- Premixed insulin combines rapid or short-acting insulin with intermediate-acting insulin. The onset, peak and duration will differ depending on the insulins used in the mix. Before injecting premixed insulin, gently shake it to re-suspend the insulin.
Some people mix two types of insulin together in a syringe before injection. Keep in mind that only a few insulins can be mixed together safely. Your primary health care provider, diabetes educator or pharmacist can provide more information about mixing insulins.
| Type of insulin | Onset of action1 | Peak of action1 | Duration of action1 |
|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1Consider these times to be estimates only. Insulin action may vary in different people and at different times in the same person. 2The first number is the percentage of short-acting insulin, the second is the percentage of intermediate-acting (NPH) insulin. For instance, Humulin 30/70 is 30 per cent regular (short-acting) insulin and 70 per cent NPH insulin. 3Humalog Mix 25 is a mixture of 25 per cent lispro insulin (rapid-acting insulin) and 75 per cent lispro protamine insulin (intermediate-acting insulin). Humalog Mix 50 combines 50 per cent lispro insulin and 50 per cent lispro protamine insulin. 4NovoMix 30 is a mixture of 30 per cent aspart insulin (rapid-acting insulin) and 70 per cent aspart protamine insulin (intermediate-acting insulin). | |||
Injecting insulin
Insulin injections have never been easier or less painful. Today’s thinner needles cause little pain when inserted through the skin. Using an insulin pen can make injections less noticeable in public. Pens are also much easier to use than vials and syringes. If you currently use syringes for injection, talk to your pharmacist or diabetes educator about the benefits of using an insulin pen.
Steps for injecting insulin
Wash your hands with warm water and soap.
If you are using a cloudy insulin such as NPH or a premix, gently shake it to re-suspend the insulin before injection. To get an even mixture, roll the vial or penfill between your hands and turn from end to end at least 20 times. It is important not to shake the vial or penfill too hard, as this can damage the insulin.
To prepare an insulin pen, dial up two units of insulin and shoot it into the air. This removes any air from the penfill and checks that your pen is working. Next, dial up the dose that you need.
To prepare a syringe, first inject the same amount of air as your insulin dose into the vial while it is right-side up. With the syringe still in the vial, turn the bottle upside down and draw up about five units of insulin. Push this insulin back into the bottle to get rid of any small air bubbles. Do this once or twice, until you can see that there are no bubbles. Next, draw your insulin dose into the syringe.
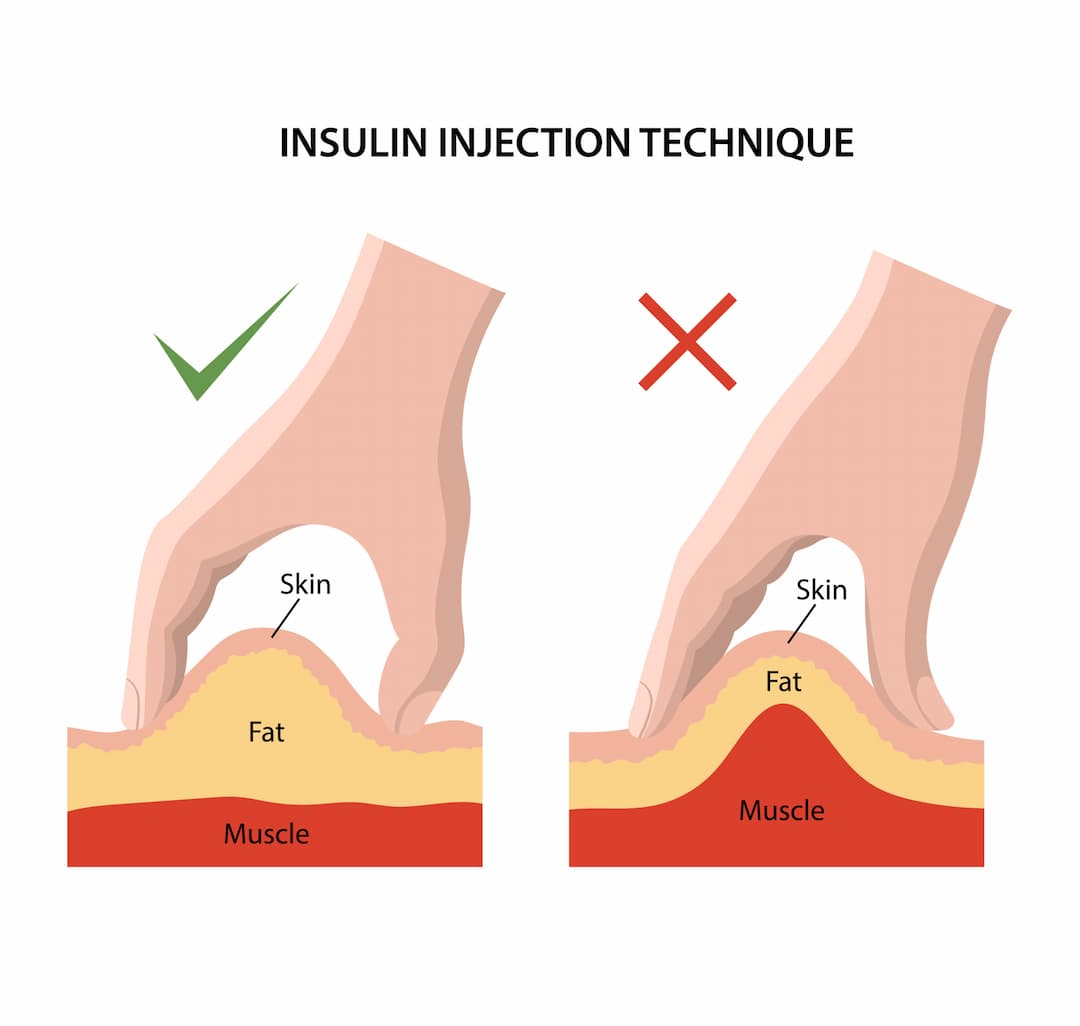
- If you are using a pen needle six millimeters in length or less, insert the needle straight into the skin at a 90-degree angle. When using a syringe or longer pen needle (eight mm or longer), you will need to pinch up a fold of skin before inserting the needle.
- Inject the insulin. Keep the needle in the skin for ten seconds before removing.
Where to inject insulin
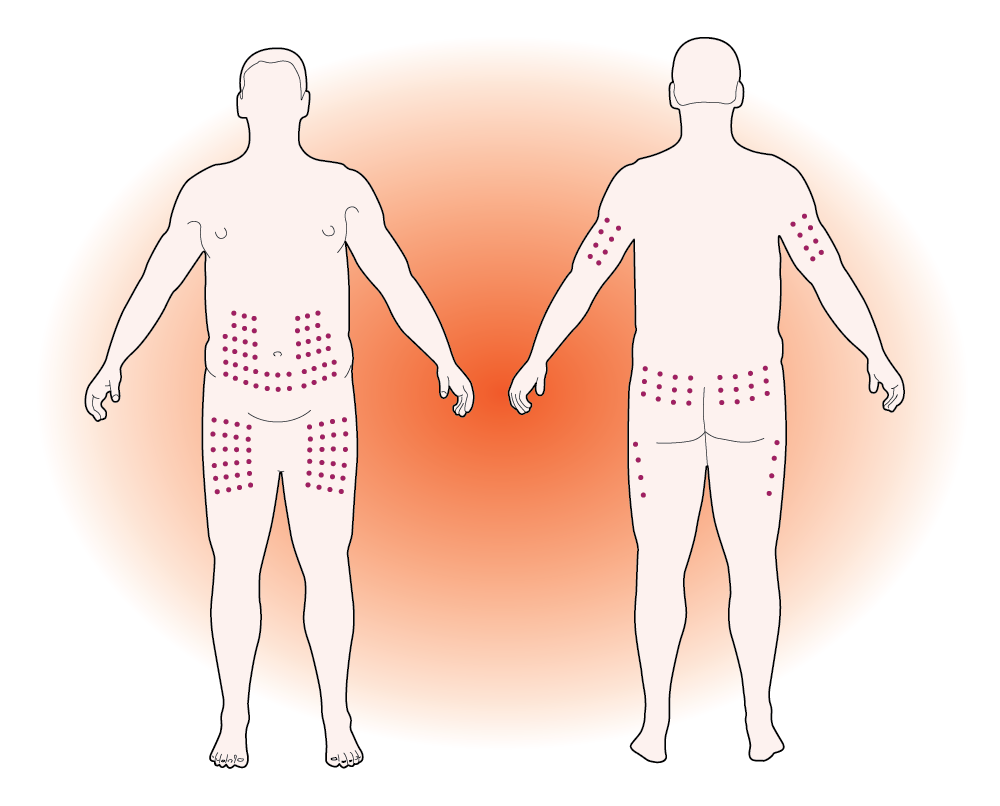
Four different areas on the body are good places to inject insulin:
- the back of the upper arms (this area is harder to self-inject)
- the abdomen
- the front and outer thighs
- the buttocks.
These sites all have a layer of fat under the skin (called subcutaneous fat) that allows insulin to be correctly absorbed by the body.
Insulin will be absorbed at a different speed in each area. The abdomen is quickest to absorb insulin. Arms, thighs and buttocks all absorb it at a slower speed. Your primary health care provider or diabetes educator can advise whether you should avoid any of these areas, or if certain locations will work better for you.
Heat, strenuous activity, and massage can all affect how quickly insulin is absorbed. If you plan to exercise after an injection, avoid injecting those areas you will be using. For instance, do not inject into your arm if playing tennis is your next activity. Note that time in the sun, a warm bath and sitting in a hot tub also influence the effect of insulin. Do not massage the injection site after injecting insulin, as this makes the insulin absorb faster.
Rotating injections
Choose a different spot to inject insulin each time. If insulin is injected into the same spot over and over, fat can build up under the skin. This lump of fat, called lipohypertrophy, can make it harder for insulin to absorb properly.
Each injection should be about 2.5 centimeters (one inch, or the width of two fingers) away from the last. Scars, moles, and the navel (belly button) absorb insulin poorly. Do not inject within five centimeters (two inches) of these areas. If you have any questions about rotating injections, talk to your diabetes care team.
Storing insulin
Insulin is delicate. If it is not handled correctly, insulin can lose its effectiveness. Take special care to keep it safe. It should not be overheated, exposed to sunlight, frozen or roughly shaken. Damaged insulin may not be able to control your blood glucose levels.
Storage tips
- Levemir is good for 42 days once opened. Toujeo and Tresiba are good for 56 days once opened. All other insulins are good for one month after opening.
- Keep open insulin at room temperature. If the insulin is cold, injections will be more painful. Do not store insulin pens you are currently using in the refrigerator.
- Store extra insulin in the refrigerator. Kept this way, unopened insulin can be used until the expiry date. Do not use insulin past its expiry date.
- Insulin that has been frozen, heated, or exposed to direct sunlight should be discarded.
- Do not use clear insulin that has particles in it, or cloudy insulin that does not mix properly. It may have been damaged.
Checking blood glucose
Most people using rapid-acting insulin with each meal check their blood glucose before meals and at bedtime. This allows them to know how much insulin to take with each meal, and confirm that their blood glucose is not too low before going to sleep. As well, checking blood glucose two hours after a meal shows how the body responded to the meal and helps make certain the right amount of insulin was taken.
Those who use only one daily injection of intermediate or long-acting insulin, or use premixed insulins, may need to check less often.
If you use insulin, be sure to check any time you suspect your blood glucose levels may be low. Ask your diabetes educator, primary health care provider or pharmacist about the best times to check your blood glucose.
Hypoglycemia (low blood glucose)
A blood glucose level below 4.0 mmol/L is called hypoglycemia. For a person using insulin, common causes of hypoglycemia are:
- increased physical activity
- taking too much insulin
- drinking alcohol without eating
- missed or delayed meals or snacks
- eating too little food.
If your blood glucose is low, you may feel weak, hungry or nauseous. You may also experience clumsiness, trembling, confusion, tingling lips, or begin to sweat.
Emergency care: managing hypoglycemia (low blood glucose)
If you think you have hypoglycemia, act quickly.
- Check your blood glucose. If this is not possible, treat yourself anyway.
- Eat or drink 15 grams of fast-acting carbohydrate. For instance, use one of the following:
- four Dex4 tablets
- ¾ cup (175 ml) of orange juice or regular soft drink
- three teaspoons (15 ml) of honey.
- After 15 minutes, check your blood glucose again. If it is still below 4.0 mmol/L, treat again with another 15 grams of fast-acting carbohydrate.
- Once your blood glucose is above 4.0 mmol/L, go ahead with your normal meal or snack if it is planned within the hour. If your next meal is more than an hour away, eat a snack. Include 15 grams of carbohydrate and a protein source, such as six crackers with peanut butter or cheese, or half of a sandwich with a protein filling.
If you have questions about how to recognize, treat or prevent low blood glucose, talk to a member of your diabetes care team.
Since insulin was discovered by Canadian doctors Banting and Best in 1921, it has been saving and improving the lives of people with diabetes. Further advances have made it more effective, safer, and easier to use. Without insulin, the body cannot create the energy required to survive. With education and training, anyone with diabetes can use this lifesaving treatment.
WRITTEN BY: Rami Chowaniec, BSc Pharm, CDE, a pharmacist and diabetes educator practicing at Southgate Safeway Pharmacy in Edmonton, Alberta.


